CLASSIFICATION OF PERIPHERAL NEUROPATHIES
There are more than 100 types of peripheral neuropathy, based on their symptoms and prognosis[3]
Peripheral neuropathy is one of the most common neurological conditions. Currently, more than 100 types of peripheral neuropathy have been defined, based on their symptoms and prognosis[3].
Peripheral neuropathies are generally classified according to the type of nerve damage[3].
Mononeuropathy
Some forms of neuropathy involve damage to a single nerve.
Polyneuropathy
More often, several nerves are affected.
How does the nerve react to injury?
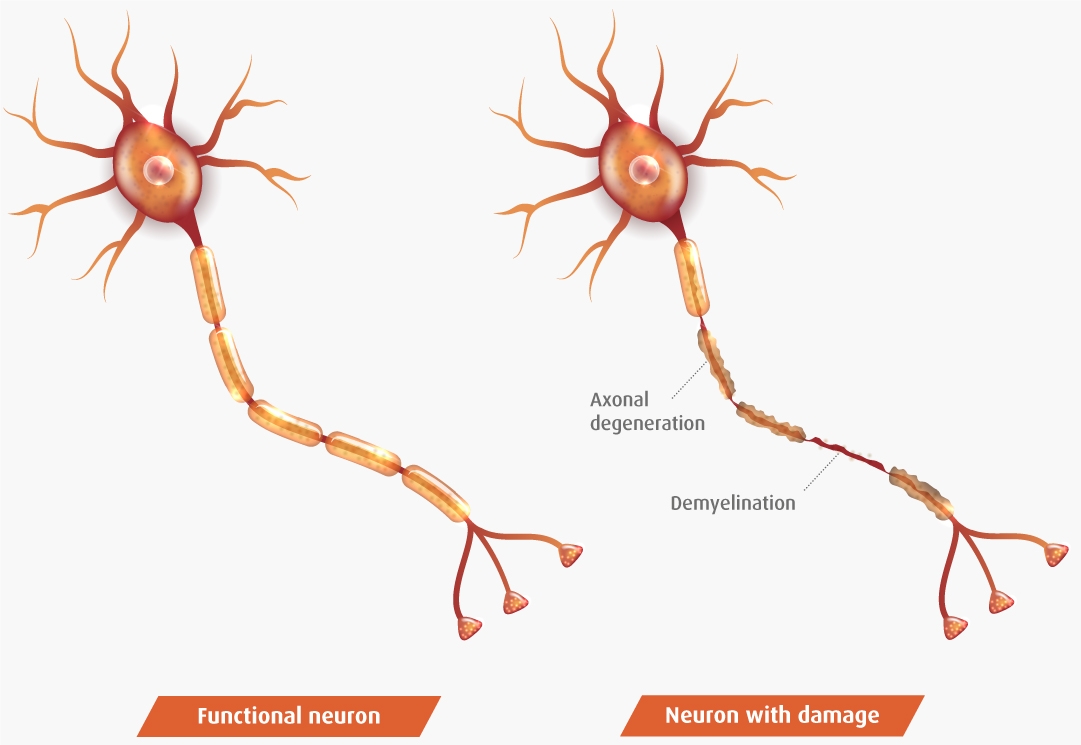
The possible reactions of nerves to these injuries are[4]:
- Axonal degeneration: some peripheral neuropathies are due to damage to nerve cell axons. In this case, the myelin sheaths surrounding the axons degenerate secondarily.
Recovery will depend on the regeneration of the axons, which is why it is slow and often incomplete.
- Demyelination: the myelin layer degenerates in a primary way, usually with preservation of the axons. In this case, there is a slowdown of nerve conduction, or even a blockage.
When re-myelination (myelin regeneration) occurs, nerve function usually recovers quickly and completely.
Did you know that peripheral neuropathy is one of the most common neurological conditions encountered by doctors of all specialties?[5]
In the current context, with an increasingly ageing population and a progressively higher incidence of diabetes and obesity, the prevalence of peripheral neuropathy is increasing, which is a major public health problem[6].

Find out the main causes of peripheral neuropathy[4,9]
There are cases of peripheral neuropathy in which it is not possible to identify a known cause (between 25-46%). This is therefore called idiopathic neuropathy[10].
In all other situations, this disorder can be inherited or acquired through disease or trauma processes:

Traumatic and entrapment neuropathies are discomfort and functional limitations of certain peripheral nerves, usually as a result of compression. There can be several reasons[11]:

Tumours
One cause of nerve compression can be the formation of peripheral nerve tumours anywhere in the body. These can lead to complications such as pain, nerve damage, numbness, weakness and loss of function in the affected area[12,13].
References
12. Tumores en los nervios periféricos - Síntomas y causas - Mayo Clinic. Último acceso abril 25, 2022. https://www.mayoclinic.org/es-es/diseases-conditions/peripheral-nerve-tumors/symptoms-causes/syc-20355070
13. Brown TJ, Sedhom R, Gupta A. Chemotherapy-Induced Peripheral Neuropathy. JAMA Oncol. 2019;5(5):750-750. doi:10.1001/JAMAONCOL.2018.6771

Trauma
Peripheral neuropathy that is acquired or secondary to trauma includes acute injuries resulting from falls, road traffic accidents or sports activities. These cause injury by compressing or crushing the nerves, preventing effective communication with the brain and spinal cord[14].
Repetitive postures and strain or poor posture can also trigger entrapment peripheral neuropathy, often as a result of tasks performed in the workplace[15].
References
14. Neuropatía periférica - Síntomas y causas - Mayo Clinic. Último acceso abril 25, 2022. https://www.mayoclinic.org/es-es/diseases-conditions/peripheral-neuropathy/symptoms-causes/syc-20352061
15. Ministerio de Sanidad y Consumo. Neuropatías Por Presión.; 2000. Último acceso abril 25, 2022. https://www.sanidad.gob.es/ciudadanos/saludAmbLaboral/docs/neuropatias.pdf

Sciatica
This is a condition caused by pressure on or compression of the sciatic nerve, which manifests as swelling, weakness or numbness in the back of the affected leg. The pain is usually intermittent and involves the buttock, lower back and thigh and may extend to the foot.
The most common causes of sciatica are a herniated disc, narrowing of the spinal canal or pressure on the sciatic nerve from the piriformis muscle[16].
References
16. Domingo Sánchez F, De Barutell C, Ortiz Soler M. Neuropatía por compresión del nervio ciático: síndrome del músculo piramidal o piriforme. Neuropatía por compresión del nervio ciático síndrome del músculo piramidal o piriforme. Published online 2016:19-22. Último acceso abril 25, 2022. https://medes.com/publication/110424

Back pain
The spinal cord or its nerve extensions may become pinched as they exit the spine due to a herniated disc or a bone spur (a bony protrusion on the edges of bones)[17,18].
Pain in the lumbar region (low back pain) is often caused by herniated discs, facet arthropathy (degeneration of the cartilage in the joints connecting the vertebrae) or narrowing of the lumbar canal, leading to entrapment of the nerves in the area.
Similarly, back pain (dorsalgia) can have multiple causes, although the most common pathology causing this condition is vertebral fractures or crushing in people with osteoporosis.
References
17. Lumbago agudo: MedlinePlus enciclopedia médica. Último acceso abril 25, 2022. https://medlineplus.gov/spanish/ency/article/007425.htm
18. Peña Sagredo J, Peña C, Brieva P, Pérez Núñez M, Humbría Mendiola A. Fisiopatología de la lumbalgia. Rev Española Reumatol. 2002;29(10):483-488. Último acceso abril 25, 2022. https://www.elsevier.es/es-revista-revista-espanola-reumatologia-29-articulo-fisiopatologia-lumbalgia-13041270

Cervicobrachialgia
This is a common type of pain due to maintaining incorrect postures, a condition of the vertebrae or intervertebral discs, or a muscular problem. When this neck pain spreads to the arms, it is called cervicobrachialgia.
The most common cause of cervicobrachialgia is entrapment or compression of a spinal nerve, due to narrowing of the nerve pathways. This can lead to neck pain radiating down the arm and cause tingling and loss of strength and sensation in the arms and hands[19].
References
19. Cohen SP. Epidemiology, diagnosis, and treatment of neck pain. Mayo Clin Proc. 2015;90(2):284-299. doi:10.1016/J.MAYOCP.2014.09.008

Carpal/tarsal tunnel syndrome
Peripheral compression neuropathy causes inflammation in the tendons, muscles and ligaments, compressing the nerve pathways.
The carpal tunnel is a narrow passage or channel of ligaments and bones at the base of the hand that contains nerves and tendons. Carpal tunnel syndrome is caused by increased pressure inside the carpal tunnel due to thickening or swelling of tissues in the area, resulting in injury to the median nerve. Patients begin to feel pain in the wrist and forearm region, in addition to numbness, cramping and tingling in the thumb, index, middle and ring fingers[20].
The tarsal tunnel is a fibrous and bony passage or canal on the inside of the ankle and hindfoot that contains nerves and tendons. Tarsal tunnel syndrome occurs when the tissues surrounding the tarsal tunnel become inflamed and compress the posterior tibial nerve, causing pain around the ankle. Patients may feel burning or tingling when standing or walking, but if the disorder progresses, the pain may also be experienced at rest[21].
References
20. Síndrome del túnel carpiano: MedlinePlus enciclopedia médica. Último acceso abril 25, 2022. https://medlineplus.gov/spanish/ency/article/000433.htm
21. Síndrome del tunel tarsal: MedlinePlus enciclopedia médica. Último acceso abril 25, 2022. https://medlineplus.gov/spanish/ency/article/000792.htm
Certain multiple peripheral neuropathies are associated with endocrine and renal diseases.

Diabetic neuropathy
Is nerve damage caused by type 1 or type 2 diabetes, affecting up to half of all patients. High blood glucose levels sustained over time can damage the nerves, as well as the small blood vessels that supply the nerves with oxygen and nutrients.
Symptoms of this neuropathy can lead to foot complications, such as sores, ulcers and infections (in severe cases they may even lead to amputation); patients may lose sensation in this vital part of the motor system, experiencing impaired balance and coordination[22].
References
22. ¿Qué es la neuropatía diabética? | NIDDK. Último acceso abril 25, 2022. https://www.niddk.nih.gov/health-information/informacion-de-la-salud/diabetes/informacion-general/prevenir-problemas/neuropatias-diabeticas/que-es

Renal or uraemic neuropathy
Has an as yet unknown cause, although hyperkalaemia (elevated blood potassium) due to a decline in kidney function may play an important role in its origin[23]. This type of neuropathy therefore appears to be the most frequent neurological complication in patients with chronic kidney disease (CKD)[19], with 50% of patients with CKD reporting pain
Patients with this neuropathy initially complain of sensory disturbances (tingling, itching) affecting the distal part of the lower limbs. When neurological damage is more advanced, motor disturbances may develop[24].
References
19. Cohen SP. Epidemiology, diagnosis, and treatment of neck pain. Mayo Clin Proc. 2015;90(2):284-299. doi:10.1016/J.MAYOCP.2014.09.008
23. Arnold R, Pussell BA, Howells J, et al. Evidence for a causal relationship between hyperkalaemia and axonal dysfunction in end-stage kidney disease. Clin Neurophysiol. 2014;125(1):179-185. doi:10.1016/J.CLINPH.2013.06.022
24. Dolores Arenas M. Complicaciones por Órganos y Aparatos. Published 2021. Último acceso abril 25, 2022. https://static.elsevier.es/nefro/monografias/pdfs/nefrologia-dia-173.pdf

Hepatic neuropathy
Can occur in response to various conditions that compromise normal liver function, such as cirrhosis or certain chronic liver disorders, causing dysfunction of peripheral nerves outside the brain and spinal cord[25].
References
25. Cirrosis hepática. Actualización. Farm Prof. 2012;26(4):45-51. Último acceso abril 25, 2022. https://www.elsevier.es/es-revista-farmacia-profesional-3-articulo-cirrosis-hepatica-actualizacion-X0213932412502272

Hypothyroid neuropathy
Is a peripheral neuropathy caused by severe hypothyroidism. Hypothyroidism involves fluid accumulation and retention, causing tissue swelling and compression on peripheral nerves.
The initial manifestations are sensory (tingling, pain), followed by motor symptoms[26].
References
26. Hipotiroidismo: ¿puede causar una neuropatía periférica? - Mayo Clinic. Último acceso abril 25, 2022. https://www.mayoclinic.org/es-es/diseases-conditions/peripheral-neuropathy/expert-answers/hypothyroidism/faq-20058489

Nutritional neuropathies
Manifest themselves acutely, sub-acutely or chronically and are caused by malnutrition; they can affect all areas of the nervous system[27].
Certain deficiencies of essential vitamins and minerals cause polyneuropathy, e.g. deficiencies of vitamin B12 (cobalamin), vitamin B1 (thiamine), copper and vitamin E (α-tocopherol).
References
27. Hammond N, Wang Y, Dimachkie MM, Barohn RJ. Nutritional Neuropathies. Neurol Clin. 2013;31(2):477. doi:10.1016/J.NCL.2013.02.002
Inflammatory neuropathies are a diverse group of diseases caused by the patient’s own immune system attacking the peripheral nerves (autoimmune disease).
These neuropathies can be acute or chronic and have varying levels of severity, including:
Acute
Guillain-Barré syndrome
A polyneuropathy affecting many peripheral nerves in the body, where the immune system attacks the myelin sheath, the axon or both. It may follow a mild viral infection, vaccination, trauma or surgery.
Symptoms, such as tingling, numbness or weakness, usually start in the legs and progress to the arms (in 10% of cases, symptoms start in the arms or face).
As Guillain-Barré syndrome progresses, muscle weakness can progress to paralysis and, in severe cases, the facial and swallowing muscles weaken; the peak of weakness occurs about two weeks after the onset of symptoms[28].
References
28. Síndrome de Guillain-Barré - Síntomas y causas - Mayo Clinic. Último acceso abril 25, 2022. https://www.mayoclinic.org/es-es/diseases-conditions/guillain-barre-syndrome/symptoms-causes/syc-20362793

Chronic
Sjögren’s syndrome
An autoimmune condition affecting the glands that produce tears and saliva. It is often linked to other immune system disorders, such as lupus or rheumatoid arthritis.
Generally, people over the age of 40 suffer from this syndrome and it is more prevalent among women.
This disease causes dry eyes and its cardinal symptoms are a feeling of having grit in the eyes, burning or itching, and a dry mouth (difficulty swallowing or speaking). However, joint pain, skin rashes, vaginal dryness, dry cough and fatigue, among others, may also occur[29].
References
29. Síndrome de Sjögren - Síntomas y causas - Mayo Clinic. Último acceso abril 25, 2022. https://www.mayoclinic.org/es-es/diseases-conditions/sjogrens-syndrome/symptoms-causes/syc-20353216
Chronic
Chronic inflammatory demyelinating polyradiculoneuropathy (CIDP)
Clinically heterogeneous disease caused by damage to the myelin sheath of peripheral nerves. It is characterised by progressive weakness and symmetrically impaired sensory function in the legs and arms.
It is most common in young adults and is more common in men than in women. In adults, a prevalence of 1-2 per 100,000 people has been documented.
The course of the disease is variable, and an acute attack of CIDP may be followed by spontaneous recovery or there may be a recurrent pattern (relapses and recoveries). It is distinguished from Guillain-Barré syndrome by the fact that it evolves over 8 weeks.
Symptoms include flaccid weakness of the legs and arms, partial or complete loss of deep tendon reflexes and abnormal sensory sensations (tingling, numbness)[30].
References
30. Castro Macias J, Briceño González E. Polirradiculoneuropatía crónica inflamatoria desmielinizante. Arch Neurocien. 2007;12(4):221-228.

Chronic
Multifocal motor neuropathy
An autoimmune condition affecting demyelination of peripheral nerves with a prevalence of 0.2-2 per 100,000 people.
It is characterised by progressive, asymmetrical weakness in the distal portion of the limbs, with varying degrees of muscle atrophy, although sensory impairment is not significant.
Symptoms occur in the arms and may be accompanied by cramps and decreased or absent stretch reflexes[31].
References
31. Chiquete E, Vargas-Cañas E, Plascencia Álvarez N, et al. Recomendaciones sobre el diagnóstico y tratamiento de la neuropatía motora multifocal. Rev Mex Neurocienc. 2018;19(1):1-22. Último acceso abril 25, 2022. http://previous.revmexneurociencia.com/articulo/recomendaciones-sobre-el-diagnostico-tratamiento-de-la-neuropatia-motora-multifocal/
Infectious neuropathies are those caused by a virus (Cytomegalovirus, Herpes simplex, Herpes zoster, Hepatitis C, Hepatitis B, HIV type 1) or by bacteria or parasites (Borrelia burgdorferi, Corynebacterium diphtheriae, Mycobacterium leprae, Trypanosoma cruzi)[32]

Human Immunodeficiency Virus (HIV)
Peripheral neuropathy is a common feature of HIV infection and is present in up to 30% of patients in late stages of the disease[33].
In HIV-infected patients, pain can be caused by the disease itself, by concomitant infections, by side effects of antiretroviral drugs or by non-HIV-related processes such as substance abuse[34].
The main symptoms are distal dysesthesias (unpleasant and often painful sensations), paresthesias (irritative-type sensitivity disorder) and numbness, initially in the lower extremities. Muscle weakness appears in late stages of the disease.
References
33. Benavides E, Soza M. Neuropatías asociadas al síndrome de inmunodeficiencia adquirida. 2003. Último acceso abril 25, 2022. http://publicacionesmedicina.uc.cl/cuadernos/2004/NeuropatiasAsociadas.html
34. Lana R, Lérida A, Mendoza J. Tratamiento del dolor neuropático en el enfermo con infección por el VIH. Enferm Infecc Microbiol Clin. 2008;26(6):348-355.

Leprosy
Leprosy neuropathy is the result of asymmetric involvement of the superficial nerves by Mycobacterium leprae, causing neuritis and compression of the peripheral nerves of the upper and lower limbs.
The nerves most affected by M. leprae are those located close to the skin, compromising the perception of external stimuli such as temperature, pain and touch[35].
As the disease progresses, the motor nerves supplying the muscles of the eyes, hands and feet become involved, and the first signs of motor impairment and progression of disability become evident. This disease negatively affects the quality of life of more than 4 million people worldwide[35].
References
35. Serrano Coll H, Cardona Castro N. Neuropatía leprótica: una mirada integral de la afección periférica causada por Mycobacterium leprae. Salud Uninorte Barranquilla (Col). 2017;33(3):451-463.

Herpes
postherpetic neuropathy is the most common complication of shingles (Herpes zoster). It is therefore estimated that 10% of patients with shingles will suffer from postherpetic neuralgia, mainly affecting those over 60 years of age26[36].
This disorder affects the nerve fibres and skin, causing pain (postherpetic neuralgia) and remains long after the rash and blisters of shingles have subsided
These patients present a clinical picture characterised by the presence of four types of pain[36].
1. Constant, dull, deep, burning pain.
2. Intermittent, intense pain that travels over the entire painful area leaving the entire area hypersensitive and painful for minutes.
3. Pain on touch (tactile allodynia; virulent sensitivity to touch, even mild) or thermal contact (thermal allodynia; harmful perception of hot or cold stimuli).
4. Persistent pain to stimuli that do not produce pain under normal conditions (hyperpathia).
References
36. Redondo Fernández M, Costillo Rodríguez J, Jiménez Rodríguez M. Abordaje de la neuralgia postherpética en Atención Primaria: situación actual del tratamiento farmacológico. Med Fam Semer. 2007;33(2):80-85. doi:10.1016/S1138-3593(07)73853-4.

Hepatitis
Peripheral neuropathy associated with hepatitis virus infection.
Up to 20% of patients with chronic hepatitis B infection have extrahepatic manifestations of the infection and may have demyelinating neurological complications. In particular, inflammatory neuropathic involvement has been described, which causes motor weakness and absent reflexes. In certain cases, it may be accompanied by a mild sensory deficit[37].
Hepatitis C virus infection can cause cryoglobulinaemia, a multi-system disease caused by the deposition of circulating proteins (cryoglobulins) in the smaller blood vessels[38]. 15-20% of these patients have peripheral neuropathy.
References
37. Penagos L, Calle L, Santos Ó. Manifestaciones extrahepáticas de la infección por el virus de la Hepatitis B. Rev Col Gastroenterol. 2016;31(3):283-287.
38. García Buey L, García Monzón C. Hepatitis C. GH Contin. 2001;1(2):64-69.
Chagas disease
A potentially fatal disease caused by the Trypanosoma cruzi parasite, which is endemic in 21 countries in the Americas and affects an estimated 6 million people in the region[39].
The initial phase of the disease involves absent or mild symptoms, while in the chronic phase the parasites remain hidden, mainly in the heart and digestive muscle. This can cause cardiac disorders and digestive (enlargement of the oesophagus or colon), neurological or mixed disorders[40].
In the majority of patients, the neurological examination is normal, although in about 11% of cases peripheral nervous system disturbances directly related to neuropathy may occur[41].
References
39. Enfermedad de Chagas - OPS/OMS | Organización Panamericana de la Salud. Último acceso abril 25, 2022. https://www.paho.org/es/temas/enfermedad-chagas
40. Organización Mundial de la Salud. La enfermedad de Chagas (tripanosomiasis americana). Último acceso abril 25, 2022. https://www.who.int/es/news-room/fact-sheets/detail/chagas-disease-(american-trypanosomiasis)
41. Duque Montoya D, Ospina Ríos J. Enfermedad de Chagas y sus manifestaciones neurológicas. Acta Neurol Colomb. 2021;37(1):154-162.

Lyme disease
a tick-borne infection caused by bacteria of the genus Borrelia. Its first symptoms are a small red bump, often at the site of the bite, which can progress, weeks or months later, to neurological, cardiac or joint problems[42].
Severe, superficial, burning, neuropathic pain has been described among the spectrum of neurological clinical manifestations of Lyme disease. There is often hyperpathia (persistent pain to stimuli that do not produce pain under normal conditions) and alterations in sensation, strength and deep tendon reflexes.
References
42. Enfermedad de Lyme - Síntomas y causas - Mayo Clinic. Último acceso abril 25, 2022. https://www.mayoclinic.org/es-es/diseases-conditions/lyme-disease/symptoms-causes/syc-20374651

Syphilis
Syphilis is a disease caused by Treponema pallidum and is mainly transmitted sexually.
There are three different stages to the disease[43]: primary syphilis (immediately after infection, with painless ulcerations on the affected skin), secondary syphilis (lesions distributed throughout the body, with swollen lymph nodes, headache and fever) and tertiary syphilis (final stage of the disease about 20 years after infection, with cardiovascular and neurological complications)[44].
Symptoms of late syphilitic neuropathy are associated with eye disorders (decreased visual acuity, impaired perception of stimuli), motor disorders that impair movement (abnormal gait, inability to walk) and loss of coordination in the limbs (numbness)[43].
References
43. Pereira D. Neurosífilis: síntomas, diagnóstico y tratamiento. Último acceso abril 25, 2022. https://infotiti.com/2018/05/neurosifilis/
44. US Preventive Services Task Force. Guía de Actividades Preventivas En La Práctica Médica. (Diaz de Santos SA, ed.).; 1992.

Toxic neuropathies occur as a consequence of multiple factors associated with environmental exposure, heavy metals, medication, comorbidities and adverse effects of drug treatments that patients undergo. They account for only 2-4% of neuropathies[45]

Drugs
Drug-induced peripheral neuropathy usually presents as a sensory-predominant polyneuropathy (paresthesias and sensory loss), which may be accompanied by distal pain[46].
Demyelination of the affected peripheral nerves may be observed and may sometimes be associated with axonal degeneration.
Symptoms may begin weeks or months after treatment begins or even after it has ended. Some of the causative agents of neuropathy of pharmaceutical origin include certain microbial agents, antifungal agents, antiretrovirals, cardiovascular drugs, immunosuppressants and chemotherapeutic agents[47].
References
46. Karam C, Dyck PJB. Toxic Neuropathies. Semin Neurol. 2015;35(4):448-457. doi:10.1055/S-0035-1558977
47. Departamento de Medicina del Dolor y Paliativa - INCMNSZ. Revisión bibliográfica: Neuropatías tóxicas. Último acceso abril 25, 2022. http://www.dolorypaliativos.org/art51.asp

Alcohol
Peripheral neuropathy is nerve damage as a result of alcohol consumption. It is estimated that this neuropathy is estimated to affects 25-66% of patients with chronic alcoholism, causing sensory, motor and autonomic dysfunction[48].
The exact cause of alcoholic neuropathy is unknown. It probably includes both the direct neurotoxic effect of alcohol and its toxic metabolites (e.g. acetaldehyde) and the effect of poor nutrition associated with alcoholism.
The most common symptoms are numbness, tingling, cramps and muscle weakness, usually in a symmetrical pattern on both sides of the body and most commonly in the lower limbs. In severe cases, the autonomic nerves (regulators of internal bodily functions) may be involved[49].
References
48. Domínguez Carrillo L, Arellano Aguilar G. Neuropatía alcohólica. Acta méd Grup Ángeles. 2018;16(2).
49. MedlinePlus Enciclopedia Médica. Neuropatía alcohólica. Último acceso abril 25, 2022. http://www.funsepa.net/medlineplus/spanish/ency/article/000714.htm

Chemotherapy
Chemotherapy-induced peripheral neuropathy is a side effect of these anti-cancer drugs and affects about one third of patients.
This neuropathy impairs functionality and compromises quality of life, which may lead to dose reduction and/or premature discontinuation of treatment[50].
The toxicity of these drugs often leads to peripheral nerve damage, causing axonal atrophy and demyelination[51]. Their effect on sensory nerves causes symptoms such as numbness, tingling, sharp or burning pain and balance problems, while involvement of motor nerves causes muscle weakness in the upper and lower limbs.
References
50. Velasco R, Bruna J. Neuropatía inducida por quimioterapia: un problema no resuelto. Neurología. 2010;25(2):116-131. doi:10.1111/cns.13207.
51. Prevalencia de neuropatía periférica asociada a quimioterapia en cuatro centros oncológicos de Colombia. Neurología.com. Último acceso abril 25, 2022. https://www.neurologia.com/articulo/2019035
Hereditary neuropathies include various congenital degenerative peripheral neuropathies that can affect sensory (sensory processing), motor (voluntary movements) and autonomic (involuntary body functions) abilities.

Charcot-Marie-Tooth disease
The most common inherited neuromuscular disease, with a prevalence of 17-25 per 100,000 people[52].
It involves damage or destruction of the myelin sheath of the nerve fibres that control muscle movement and those that transmit sensory information to the brain.
Symptoms usually begin in adolescence, usually with foot problems such as cavus foot (pronounced arch) or hammertoes. Motor neuropathy progressively affects the upper and lower limbs symmetrically, resulting in weakness and atrophy of the hand and foot muscles, claw hand and equine gait (walking on tiptoes), among other effects[52].
Those affected also lose sensory abilities, such as feeling vibration, pain and temperature.
References
52. Vargas Cañas AM, Poblete C, Laso J. Enfermedad de Charcot-Marie-Tooth en el diagnóstico diferencial de la neuropatía craneal múltiple. Neurol Argentina. 2019;11(4):233-240. doi:10.1016/J.NEUARG.2018.10.002

Hereditary neuropathy with liability to pressure palsies (HNPP)
An inherited neuropathy with susceptibility to recurrent, painless episodes of peripheral paralysis caused by low-intensity trauma or compressive processes. Global prevalence estimates range from 1/50,000 to 1/20,000[53]
In HNPP, the myelin of the affected peripheral nerves is damaged, which become progressively more sensitive to pressure and stretching. Usually only a single nerve is involved (mononeuropathy), but several nerves can be affected at the same time (polyneuropathy), and even all four limbs simultaneously.
The symptoms of peripheral paralysis vary widely, ranging from mild to severe and lasting from minutes to months. Injured areas are usually places with a tendency to compression and where the nerve is more vulnerable (e.g. carpal tunnel, head of the fibula)[54].
References
53. Orphanet: Neuropatía hereditaria con susceptibilidad a la parálisis por presión. Último acceso abril 25, 2022. https://www.orpha.net/consor/cgi-bin/OC_Exp.php?lng=es&Expert=640
54. Díaz Negrillo A. Neuropatía hereditaria con susceptibilidad a la parálisis por presión. Estudio clínico, neurofisiológico y genético de 3 casos esporádicos. Acta Neurológica Colomb. 2014;30(4). Último acceso abril 25, 2022. http://www.scielo.org.co/scielo.php?script=sci_arttext&pid=S0120-87482014000400013
Bibliographic references
3. Neuropatía periférica | NINDS Español. https://espanol.ninds.nih.gov/es/trastornos/forma-larga/neuropatia-peri… (último acceso junio 23, 2021).
4. Casademont Pou J. Neuropatías: concepto, manifestaciones clínicas, clasificación, diagnóstico, pruebas complementarias y estrategias terapéuticas. Med - Programa Form Médica Contin Acreditado 2003;8:5373–8. doi:10.1016/s0304-5412(03)70997-4.
5. Watson JC, Dyck PJB. Peripheral Neuropathy: A Practical Approach to Diagnosis and Symptom Management. Mayo Clin Proc 2015;90:940–51. doi:10.1016/j.mayocp.2015.05.004.
6. Barrell K, Smith AG. Peripheral Neuropathy. Med Clin North Am 2019;103:383–97. doi:10.1016/j.mcna.2018.10.006.
7. Negrão L, Almeida P, Alcino S, Duro H, Libório T, Melo Silva U, et al. Effect of the combination of uridine nucleotides, folic acid and vitamin B12 on the clinical expression of peripheral neuropathies. Pain Manag 2014;4:191–6. doi:10.2217/pmt.14.10.
8. Hicks CW, Selvin E. Epidemiology of Peripheral Neuropathy and Lower Extremity Disease in Diabetes. Curr Diab Rep 2019;19:86. doi:10.1007/s11892-019-1212-8.
9. Neuropatía periférica - Síntomas y causas - Mayo Clinic. https://www.mayoclinic.org/es-es/diseases-conditions/peripheral-neuropa… (último acceso junio 23, 2021).
10. Castelli G, Desai K, Cantone R. Peripheral Neuropathy: Evaluation and Differential Diagnosis - PubMed. Am Fam Physician 2020;102:732–9.
11. Galán MGM, Alonso JJR, García HV. Neuropatías por atrapamiento. FMC Form Médica Contin en Atención Primaria. 2008;15(1):10-20. doi:10.1016/S1134-2072(08)70726-6
32. Pradilla G. Diagnóstico y tratamiento de las neuropatías periféricas Diagnóstico y tratamiento de las neuropatías periféricas. https://www.acnweb.org/guia/g5cap14.pdf (último acceso abril 25, 2022).
45. Manji H. Toxic neuropathy. Curr Opin Neurol. 2011;24(5):484-490. doi:10.1097/WCO.0B013E32834A94B6
Revised content: September 16, 2024.